Uterine Fibroids
Dr. med. Judith Kouematchoua, Obstetrician and Gynaecologist based in Hamburg, answers questions on uterine fibroids, the most common benign tumor of the uterus and one leading cause for a hysterectomy, especially among black women.
What is a fibroid?
A uterine fibroid is the most common benign (not cancerous) tumor of the woman’s uterus (womb). It is typically discovered during a woman’s middle and later reproductive years (25-50). The growths are made up of muscle and fibrous tissue that is normally found in the wall of the uterus and can vary in size. They can develop within the uterine wall itself or attach to it. They may grow as a single tumor or in clusters.
These growths occur in 40 to 50% of all women and are one leading cause of hysterectomies (removal of the uterus) especially in African/Afro-Caribbean populations. Other names for fibroids are uterine leiomyoma, myoma, fibromyoma, fibroleiomyoma.
What are the causes of fibroids? Are there risk groups?
The exact reasons why some women develop fibroids are unknown. Fibroids tend to run in families. Women of African descent are two to three times more likely to develop fibroids than women of other races.
Fibroids grow in response to stimulation by the hormone estrogen, produced naturally in the body. These growths can show up as early as age 20 and shrink after menopause when the body stops producing large amounts of estrogen.
The following factors have been associated with the presence of fibroids:
- Obesity
- Never having given birth to a child
- Onset of the menstrual period prior to age 10
- Occurring 3-9 times more often among black women than in Caucasian women
What are the symptoms?
Fibroids can be tiny and cause no problems most of the time. They also can grow to weigh several pounds. Fibroids normally grow slowly.
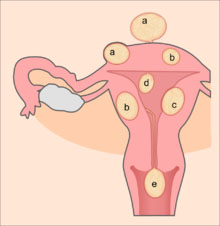
a=subserosal fibroids, b=intramural fibroids, c=submucosal fibroid, d=pedunculated submucosal fibroid, e=fibroid in statu nascendi
The following symptoms can be caused by fibroids:
- Irregular (exc essive) vaginal bleeding leading to anaemia
- Lower abdominal pain
- Pressure on the bladder, which may cause frequent urination
- Pressure on the rectum, resulting in constipation
- Pelvic pressure, “feeling full” in the lower abdomen
- Increase in size around the waist and change in (lower) abdominal shape
- Infertility which is defined as inability to become pregnant after 1 year of attempting to get pregnant.
Therapy, side effects and consequences
Most fibroids do not require treatment unless they are causing symptoms. After menopause, fibroids shrink and it is unusual for fibroids to cause problems. Treatment of fibroids depends on the symptoms, the size and location of the fibroids, the patient’s age (how close the person is to menopause), the patient’s desire to have children, and the patient’s general health.
Symptomatic uterine fibroids can be treated by:
- Hysterectomy
- Medication (to control symptoms and aimed at shrinking fibroids)
- Myomectomy
- Ultrasound fibroid destruction
- Uterine artery embolization
Myomectomy
Myomectomy is a surgical procedure to remove one or more fibroids. It is usually recommended when conservative treatment options fail, for women who want fertility preserving surgery or who express desire to retain the uterus. This can be accomplished through hysteroscopy (through the uterine cavity), laparoscopy, or an open procedure (an incision in the abdomen). The surgical approach depends on the size and location of the fibroid. Myomectomy has also been shown to have a decreased likelihood of injury to the bowel, bladder, or ureter than hysterectomy. The uterus is left intact in this type of procedure, and the patient may be able to become pregnant, although in some circumstances subsequent pregnancies can be difficult or impossible.
Hysterectomy
Hysterectomy is the classical method of treating fibroids by removing (almost) the whole uterus. It is recommended only as a last option. It is the most commonly performed surgical procedure in the treatment of fibroids and is considered as the only definitive cure. Depending on the size of the fibroid, hysterectomy can be performed with incisions through the vagina, the abdomen, or by using laparoscopy.
Magnetic resonance guided focused ultrasound (MRgFUS)
Magnetic Resonance guided Focused Ultrasound is a non-invasive intervention (requiring no incision) that uses high intensity focused ultrasound waves to destroy tissue in combination with magnetic resonance imaging (MRI), which guides and monitors the treatment. During the procedure, delivery of focused ultrasound energy is guided and controlled using MR-thermal imaging. Patients who have symptomatic fibroids, who desire a non-invasive treatment option and who do not have contraindications for MRI are candidates for MRgFUS. About 60% of patients qualify for this treatment. It is an outpatient procedure and takes one to three hours depending on the size of the fibroids. It is safe and about 75% effective. Need for additional treatment varies from 16-20% and is largely dependent on the amount of fibroids that can be safely ablated; the higher the ablated volume, the lower the re-treatment rate. There are currently no randomized trials between MRgFUS and UAE. This method of fibroid treatment is not yet widely established and only very few clinical centers in Germany offer it.
Medication
A number of medications are in use to control symptoms caused by fibroids.
- Non steroidal anti-inflammatory agents (Pain killers), such as ibuprofen, have been shown to relieve pelvic pain associated with fibroids.
- Oral contraceptive pills are prescribed to reduce uterine bleeding and cramps.
- Anaemia may have to be treated with iron supplementation.
- Levonorgestrel intrauterine devices (IUD) can be effective in limiting menstrual blood flow and improving other symptoms. Side effects are very moderate because the levonorgestrel (a progestin) is released in low concentration locally. There is evidence that Levongestrel-IUDs can provide good symptomatic relief for women with fibroids by reducing the bleeding.
- Medications aimed at shrinking fibroids like Gonadotropin releasing hormone (GnRH) agonists are only available for short term treatment (6 months) and have so far showed unpleasant side effects. Fibroids can regrow once treatment is stopped. GnRH agonists can be used prior to an operation.
- Ulipristal acetate is a synthetic selective progesterone receptor modulator which has been tested in small randomized trials with good results concerning bleeding control and shrinking of the fibroids (up to 40% of the original size) also beyond the treatment time of three months. It also showed fewer side effects than GnRH agonists. Further bigger studies will have to confirm these observations. In Germany the first fibroid treatment with Ulipristal acetate will be available mid 2012.
Uterine artery embolization (UAE)
Using interventional radiology techniques, the radiologist occludes both uterine arteries, thus reducing blood supply to the fibroid. The procedure is done by inserting a catheter (small tube) into an artery of the leg (the femoral artery), using a special X-ray video to trace the arterial blood supply to the uterus, then clotting the artery with tiny plastic or gelatin sponge particles the size of grains of sand. This material blocks blood flow to the fibroid and shrinks it. This intervention is not usually recommended when fertility should be preserved. A patient will usually recover from the procedure within a few days. The UAE procedure should result in limited blood supply to the fibroids which should prevent them from further growth and heavy bleeding. The treatment is a potential option for women with fibroids, who have completed child-bearing and want to avoid surgery, or are not good candidates for it, and/or where others methods have failed. This intervention can only be performed in specialized radiology centres.
What happens when fibroids reoccur after having gone through a major operation?
In this case, the patient has to discuss with her doctor about the same or other treatment possibilities depending on her personal situation as mentioned above.
What is your advice to young girls or women who have this condition?
Firstly, as we saw above, only a low percentage (10-20%) of women with fibroids need to treat them. Thus, the diagnosis of fibroids by chance (without any symptom) should not be a reason of concern.
Secondly it depends on the patient’s age, condition, will and family planning. It is always very important when facing a major medical problem to receive appropriate counselling from the doctor (who answers all the patient’s questions and gives her time to make decisions). If necessary the patient should seek a second opinion.
The methods of treatment presented here are established as effective ones. Apart from the hysterectomy, none of them can assure a definitive cure.
Dr. med. Judith Kouematchoua
Obstetrician and Gynaecologist
AGONMVZ
Beim Schlump 52A
20144 Hamburg
Germany
References:
Gemeinsame Stellungnahme von der Deutschen Gesellschaft für gynäkologische Endokrinologie und Fortpflanzungsmedizin (DGGEF) e.V. und dem Berufsverband der Frauenärzte (BVF) e.V. : Ulipristalacetat zur konservativen Myomtherapie und Blutungskontrolle bei Hypermenorrhoe durch Uterus Myomatosus. Frauenarzt April 2012
Pfleiderer, Breckwoldt, Martius: Gynäkologie und Geburtshilfe. Thieme Verlag 2000
www.emedicinehealth.com/uterine_fibroids/
http://en.wikipedia.org/wiki/Uterine_fibroid